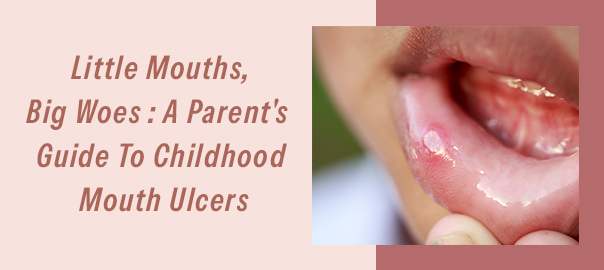
Little Mouths, Big Woes: A Parent’s Guide to Childhood Mouth Ulcers
Hey there, parents and caregivers! Today, we are tackling a topic that may have caused a few tears in your household—mouth ulcers in kids.
These excruciating sores can quickly transform mealtime into a battleground for young children and school-age children. Seeing your children suffer is painful, but we at Clove Dental are here to support you. Together, let’s dig in and solve this!
What Are Mouth Ulcers?
Small, round, whitish lesions with red borders that develop inside the mouth are called mouth ulcers, or canker sores. Usually, they show up on the inner cheeks, gums, or tongue.
Even though these ulcers are usually not harmful, they can be extremely uncomfortable.
This guide covers everything you need to know, from symptoms to home remedies, and even when it’s time to consult a dentist.
Key Characteristics:
- Size: Small to medium
- Appearance: Whitish or yellowish center with a red rim
- Location: Inside cheeks, tongue, gums, or inner lips
- Contagiousness: Usually not contagious
Common Causes: Why Do Mouth Ulcers Appear?
Mouth ulcers can have multiple triggers, and identifying the cause is key to treatment.
Common Causes:
- Injuries: Accidental cheek bites or burns from hot food.
- Nutritional Deficiencies: Lack of vitamins like B12, folic acid, or iron.
- Stress: Emotional or physical stress, such as starting school.
- Food Sensitivities: Spicy or acidic foods.
- Infections: Viral infections like hand, foot, and mouth disease.
Comparison Table of Mouth Sores
| Type | Appearance | Contagious | Common Causes |
|---|---|---|---|
| Canker Sores | Round, whitish with red edges | No | Stress, injuries, deficiencies |
| Cold Sores | Blisters on lips or mouth | Yes | Herpes simplex virus |
| Hand, Foot & Mouth | Sores with rash on hands/feet | Yes | Coxsackievirus |
| Injury-Related Sores | Red spots, inflamed edges | No | Burns, bites, sharp snacks |
Signs and Symptoms
Knowing the symptoms can help you identify a mouth ulcer quickly and take appropriate action.
1. Pain: Intense discomfort, especially while eating or speaking.
2. Swelling: Inflammation around the ulcer.
3. Difficulty Eating or Drinking: Avoidance of meals or liquids due to pain.
4. Recurring Ulcers: Frequent appearances may indicate an underlying issue.
Home Remedies for Relief
When these sores strike, here are some tried-and-tested remedies to ease the pain:
Effective Remedies:
1. Cold Foods:
Popsicles, ice cream, or chilled yogurt can numb the pain.
2. Honey:
A natural soother for ulcers (suitable for kids over one year).
3. Saltwater Rinses:
For children over five, saltwater rinses help cleanse and soothe.
4. Topical Gels:
Over-the-counter gels, as recommended by a dentist, can reduce pain.
5. Soft Foods:
Mashed potatoes, scrambled eggs, and smoothies reduce irritation.
6. Hydration:
Encourage water or diluted juice to keep them hydrated.
Prevention
Preventing mouth ulcers can save your child a lot of discomfort. Here’s how:
Good Oral Hygiene:
Teach proper brushing and flossing habits.
Balanced Diet:
Ensure sufficient intake of iron, vitamin B12, and folic acid.
Avoid Trigger Foods:
Limit acidic or spicy foods.
Stress Management:
Encourage activities like drawing or storytelling to alleviate anxiety.
Cultural Sensitivity Note: In regions where traditional remedies are preferred, such as coconut oil or turmeric paste, consult with a dentist to ensure their safety and efficacy.
Age-Specific Guidance for Mouth Ulcers
Toddlers (1-3 years)
- Communication challenges make diagnosis harder
- Watch for drooling and food refusal
- Use soft-bristled toothbrushes designed for toddlers
- Consider silicon-based oral gel applicators for safer treatment
Preschoolers (3-5 years)
- Can better communicate pain locations
- Introduce fun oral care routines
- Use reward charts for maintaining oral hygiene
- Choose child-friendly flavored oral gels
School-age children (6+ years)
- Can follow mouth rinse instructions
- Understand preventive measures
- May notice triggers themselves
- Can use salt water rinses under supervision
Mealtime Strategies During Ulcer Outbreaks
Food Temperature Tips:
- Serve room-temperature foods
- Avoid extremely hot meals
- Cool down soups and drinks before serving
- Consider frozen yogurt or smoothies for nutrients
Smart Food Choices:
- Soft fruits like bananas and melons
- Well-cooked pasta with mild sauce
- Protein-rich smoothies
- Lukewarm soups
- Avoid crunchy snacks that might hurt
Creating an Ulcer Care Kit for Kids
Keep these items handy:
- Child-safe oral gel
- Soft-bristled toothbrush
- Cool pack for soothing
- Straw for easier drinking
- Their favorite soft snacks
- Distraction toys for treatment time
Making Treatment Fun
1. Story Time Approach
- Tell stories about “healing superheroes”
- Use positive reinforcement
- Create a treatment routine with fun elements
2. Reward System
- Stickers for taking medicine
- Small prizes for following care instructions
- Positive charts for tracking healing
School and Social Situations
Tips for Teachers:
- Inform teachers about your child’s condition
- Pack appropriate lunches
- Provide pain relief medication if needed
- Share trigger foods to avoid
Social Support:
- Help children explain their condition to friends
- Pack comfortable food for playdates
- Prepare them for questions from peers
- Build confidence despite temporary discomfort
The Silent Impact of Mouth Ulcers on Children
While mouth ulcers are minor, their impact can be significant:
Emotional Distress:
Pain can make children irritable and anxious.
Nutritional Deficiencies:
Avoiding food might lead to a lack of essential nutrients.
Social Withdrawal:
Difficulty speaking might make them shy away from peers.
Expert Tip: Keep a diary of triggers and dietary patterns to better understand the root cause of recurring ulcers.
When to See a Dentist
Consult a pediatric dentist if:
- The ulcer lasts longer than two weeks.
- It is larger than a pencil eraser.
- Your child has a fever or difficulty eating.
- Ulcers occur frequently, indicating potential underlying health issues.
Final Thoughts
Mouth ulcers, while uncomfortable, are manageable with the right care. By identifying the triggers and following proper remedies, you can alleviate your child’s discomfort.
For persistent or severe cases, consult with a pediatric dentist.
FAQs
What causes a mouth ulcer to occur?
Mouth sores can arise from injuries, stress, infections, or lack of nutrients.
What are some ways to treat an ulcer in my child’s mouth?
Utilize topical gels, soft cuisine, and home solutions such as honey or chilled foods. See a dentist for ongoing situations.
Are oral sores hazardous?
The majority are benign, but persistent or long-lasting ulcers need medical care.
What deficiency leads to mouth ulcers?
Common culprits include deficiencies in iron, folic acid, or vitamin B12.
Leave a Reply
Leave a Reply
Explore More Similar Posts
Explore More Blogs


Leave a Reply